A priority for all health innovation networks, a focus for specific projects
The safety of patients is a critical thread running throughout all of our programmes of work.
In addition, we deliver patient safety specific programmes covering a multitude of care settings including acute care, maternity and neonatal units, mental health trusts, primary care, community and care homes. These all link to the NHS England National Patient Safety Improvement programme, which focuses on improving the safety of patients across systems.
A strategy for safety
Our health innovation networks and the Patient Safety Collaboratives (PSCs) they host are making an important impact on the NHS’s Patient Safety Strategy. This is down to the PSCs’ work supporting National Patient Safety Improvement Programme delivery and focus on encouraging the spread and uptake of innovation.
Patient safety in partnership: Our plan for a safer future 2019-2025 has been developed in line with the NHS Patient Safety Strategy , published in 2019, detailing how we aim to work more closely with health and care organisations to improve safety in both hospitals and community-based services.
Patient Safety Collaboratives
PSCs are funded and nationally coordinated by NHS England and hosted locally by regional health innovation networks.
The PSCs are making their impact by identifying and rolling out safer care initiatives within the NHS and industry, ensuring these are shared throughout the health and care system.
To do so, they deliver the National Patient Safety Improvement Programmes (NatPatSIP) – a key part of the NHS Patient Safety Strategy – collectively forming the largest safety initiative in the NHS in its near century-long history.
The PSC teams are experts in supporting quality improvement projects using the Institute of Healthcare Improvement (IHI) model for improvement. Download the PSC quality improvement resource pack to find out more.
NatPatSIP aims

The core objective of the programmes is to support NHS organisations in adopting safety interventions and strategies, learn from excellence, and to support systems to continually improve – continually reducing error, harm and death, to make the NHS comparable with the safest health care services in the world by 2025.
Each PSC works with its local Integrated Care System (ICS) to develop and distribute innovative improvement methods, which are systematic, evidence-based and measurable.
The NatPatSIP’s current work focuses on five safety improvement programmes (download the driver diagram below):
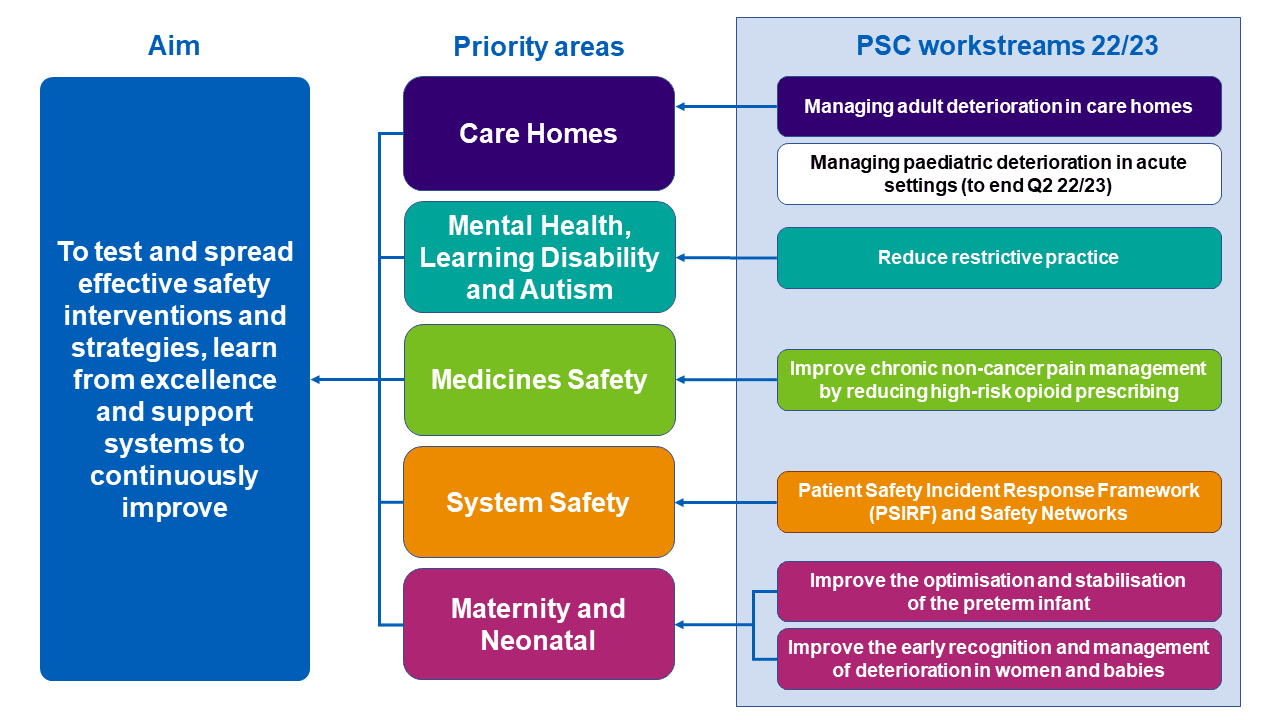
Care home safety
Together, we will reduce deterioration-associated harm by improving the planning, identification, escalation and response (PIER) to physical deterioration by March 2023.
Maternity and neonatal safety
Together, we will improve the safety and outcomes for all women, babies, and families across maternity and neonatal care settings in England.
Medicines safety
Together, we will reduce the severe harm and death associated with medicines by 50% over five years.
Mental health, learning disability and autism safety
Together, we will improve safety by reducing harm caused to people using mental health, learning disabilities and autism in-patient services by 2023.
System safety
Together, we will create optimal conditions for patient safety improvement across systems.
Key enablers
The delivery of the five safety programmes is shaped by key enablers:
- Patient and staff co-development
- Achieving patient safety equity
- Positive safety climate and culture
- Transformational improvement leadership
- Building effective patient safety and quality improvement capacity and capability
Get in touch
Contact your local health innovation network patient safety team to access support or more information on the safety programmes.



